In recent years, growing awareness about Apraxia of Speech has led to more questions from concerned parents and caregivers. Understandably, when a child struggles with speaking clearly or consistently, it becomes a source of stress and uncertainty for families. However, advancements in paediatric neurology and speech sciences are shedding new light on this complex condition.
In this blog, we’ll explore the latest findings on Apraxia of Speech, its causes, diagnosis, and the evolving landscape of treatment approaches—especially the big question: can it truly be cured?
Understanding Apraxia of Speech
To begin with, Apraxia of Speech (AOS), particularly childhood apraxia, is a motor speech disorder. It doesn’t result from muscle weakness or paralysis; instead, it originates from the brain’s difficulty in planning and coordinating the movements needed for clear speech.
This condition is especially tricky because children may know what they want to say but can’t get the words out correctly or consistently. Moreover, symptoms can vary widely from child to child, making diagnosis a nuanced process.
Key Characteristics and Early Signs
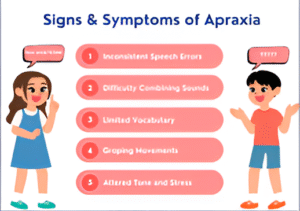
Although symptoms may overlap with other speech disorders, there are some defining traits of Apraxia of Speech that experts look for:
-
Inconsistent sound errors during repeated speech attempts
-
Difficulty stringing together syllables in the correct order
-
Groping movements of the mouth when trying to speak
-
Better speech clarity during automatic or memorized phrases than in spontaneous speech
Consequently, these symptoms can be subtle at first, but over time, they become more noticeable, especially as children begin to form sentences.
What Causes Apraxia in Children?
The causes of Apraxia of Speech in children can be diverse. In some cases, it may be linked to neurological conditions, genetic syndromes, or brain injuries. However, in many instances, the exact cause remains unclear.
Nevertheless, ongoing research in paediatric neurology is beginning to uncover potential contributing factors:
-
Genetic markers possibly affecting brain development
-
Neurological immaturity, which delays proper motor coordination
-
Family history of speech or learning disorders
Despite these findings, every case is unique. Therefore, accurate diagnosis is crucial before beginning any form of therapy.
Diagnosing Apraxia: A Team Effort
Identifying Apraxia of Speech involves a detailed, multi-disciplinary approach. While a speech-language pathologist plays a central role, paediatric neurologists, developmental pediatricians, and psychologists may also contribute to the assessment.
Here’s what the diagnostic process typically includes:
-
Speech evaluation to analyze sound production and coordination
-
Language testing to assess comprehension and vocabulary
-
Neurological exam to rule out other motor or developmental disorders
-
Observation over time to note patterns and inconsistencies
Because the symptoms can mimic other speech delays or disorders, such a thorough approach ensures that children receive the correct diagnosis and treatment plan.
Can It Be Cured?
This is, by far, the most common and pressing question for families: Can Apraxia of Speech be cured?
The short answer is not exactly, but there’s more to the story.
Unlike a cold or infection, Apraxia of Speech isn’t something that disappears entirely after treatment. Instead, it’s considered a condition that can significantly improve over time with the right interventions. As therapy progresses, many children make remarkable gains in communication, although some may continue to experience residual difficulties.
Importantly, the latest insights from paediatric neurology suggest that early intervention, frequent therapy sessions, and customized strategies can dramatically improve outcomes.
The Role of Consistent and Targeted Therapy
Even though there’s no one-size-fits-all treatment, research consistently shows that frequent, personalized therapy yields the best results. Most treatment plans involve intensive speech-language therapy, with sessions multiple times per week.
Here’s what typically makes therapy effective:
-
Repetition and practice, using structured speech exercises
-
Multi-sensory cues, like visual and tactile prompts, to reinforce sounds
-
Family involvement, so that the practice continues outside the clinic
-
Progress tracking, to adapt and evolve therapy techniques as the child improves
Furthermore, therapists often use dynamic tactile and visual feedback methods that help the child “feel” and “see” how to form words correctly.
Technology and New Tools in Therapy
Thanks to modern technology, tools like speech apps, video modeling, and AI-driven pronunciation guides are making therapy more engaging and accessible. Additionally, children can now receive support even from home, especially through online platforms or hybrid therapy models.
Although technology doesn’t replace human therapy, it complements it by reinforcing concepts learned during in-person sessions.
Long-Term Outlook: What Can Parents Expect?
While the journey might be long and sometimes challenging, the prognosis for Apraxia of Speech is increasingly optimistic.
Here are some hopeful facts backed by research:
-
Many children, especially those who start therapy early, go on to speak clearly and confidently.
-
Progress might be slower compared to peers, but it can be steady and long-lasting.
-
Emotional and academic development often improve alongside speech gains.
That said, regular re-evaluations and continued support are key, especially as language demands increase with age and schooling.
Supporting Your Child Beyond Therapy
Beyond structured sessions, a nurturing environment plays a crucial role in recovery. Encouraging your child to communicate in everyday settings, without pressure, is essential.
Here are some daily practices that can help:
-
Celebrate small victories, no matter how minor they seem.
-
Read aloud together, and encourage your child to repeat words.
-
Create communication-rich routines—at mealtime, during play, and bedtime.
-
Stay patient and avoid correcting too often. Instead, model the correct pronunciation.
Ultimately, creating a safe and supportive space boosts your child’s confidence, which directly impacts speech improvement.
Conclusion: Looking Ahead with Hope
In conclusion, while Apraxia of Speech may not have a definitive cure, it has a path to improvement. Thanks to growing research, targeted therapies, and new technologies, children today have a much stronger chance at overcoming the communication challenges they face.
Furthermore, consistent involvement from both families and medical professionals is proving critical to maximizing speech therapy outcomes. When caught early and treated with dedication, the journey can transform into one of progress, resilience, and success.
Dr. Vivek Mundada, a leading consultant pediatric neurologist, emphasizes the importance of early diagnosis and personalized intervention strategies. His expertise continues to guide families through the complexities of neurological speech disorders, helping them access the best possible care.
Most importantly, as the field of paediatric neurology continues to advance, so does our understanding of effective interventions. And in places where innovation meets care, like centers for child speech development in Dubai, families can find hope, guidance, and comprehensive support every step of the way.