Introduction
Children’s brains are remarkably resilient, yet Hemorrhagic Stroke for Health remains a sudden, frightening event that can upend any family’s life. Moreover, because it involves bleeding within the brain rather than a blockage, it demands an entirely different emergency response. Consequently, understanding what triggers such strokes in young patients—and, importantly, knowing what to do in those critical first minutes—can quite literally save a life. This comprehensive guide therefore explores causes, symptoms, and immediate steps so that parents, teachers, coaches, and caregivers can react confidently and quickly.
What Exactly Is a Pediatric Hemorrhagic Stroke?
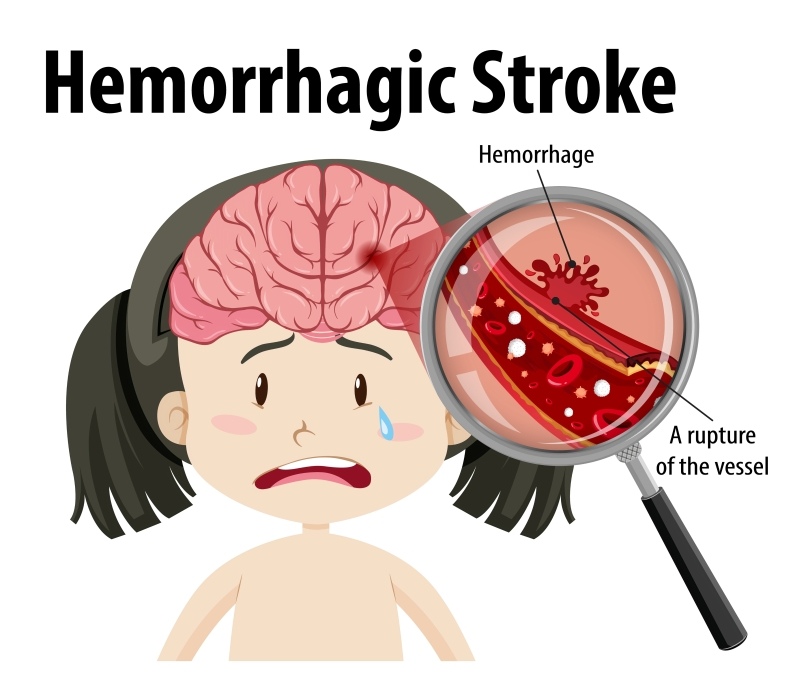
First, let’s clarify definitions. A hemorrhagic stroke occurs when a vessel inside the brain bursts, spilling blood into delicate neural tissue. Unlike adult cases, pediatric hemorrhagic events frequently stem from congenital, infectious, or traumatic factors rather than lifestyle‐related issues. Furthermore, the signs in children can be subtle or atypical, so vigilance is essential. Because Hemorrhagic Stroke for Health remains relatively rare in kids, early signs are often misattributed to migraines, seizures, or even behavioral changes—hence, timely recognition is paramount.
Underlying Causes: Why Does Bleeding Occur?
Although every child is unique, the medical literature consistently points to several high‑risk pathways. Accordingly, parents and clinicians should watch these factors closely:
-
Congenital vascular malformations (e.g., arteriovenous malformations) that, sooner or later, may rupture.
-
Blood‑clotting disorders such as hemophilia, which, consequently, allow minor bumps to become major bleeds.
-
Head trauma from falls, sports collisions, or car accidents, especially when protective gear is absent.
-
Infections like meningitis that inflame vessels until they weaken and break.
-
Neoplastic causes, including brain tumors that erode nearby arteries or veins.
Moreover, chronic hypertension in adolescents, though uncommon, can still provoke vessel rupture, while sickle‑cell disease occasionally leads to fragile cerebral vessels. Because each cause carries unique warning signs, clinicians must piece together clinical history and imaging rapidly. For this reason, discussing family medical backgrounds at routine checkups can provide invaluable clues long before Hemorrhagic Stroke for Health strikes.
Recognizing Symptoms Early—and Why Minutes Matter
Time equals brain tissue. Therefore, the moment a child exhibits unusual neurological signs, prompt evaluation is vital. Look for these red flags:
-
Sudden, severe headache, especially if described as “the worst ever.”
-
Repeated vomiting without an obvious gastrointestinal cause.
-
Weakness or numbness on one side of the face or body.
-
Seizures appearing without prior history.
-
Vision changes, such as double vision or partial blindness.
-
Difficulty speaking, slurred words, or unsteady gait.
Furthermore, irritability, loss of consciousness, or a dramatic change in school performance can, over time, indicate ongoing micro‑bleeds. Consequently, any combination of these symptoms—especially after a blow to the head—should prompt an immediate emergency call. Acting within the first “golden hour” significantly improves survival and long‑term outcomes for Hemorrhagic Stroke for Health patients.
Immediate Steps: Acting Decisively Saves Lives
Because panic often paralyzes bystanders, rehearsing a clear action plan beforehand helps ensure confidence. Therefore, if you suspect a hemorrhagic stroke:
-
Call emergency services immediately—do not drive unless professional help is unavailable, as airway compromise can occur en route.
-
Keep the child safe and still. Lay them on one side to reduce aspiration risk, and support the head gently.
-
Document the timeline. Note when symptoms began, because treatment decisions—including surgical intervention or reversal agents—depend on accurate timing.
-
Avoid food, drink, or medication (unless instructed by professionals); choking risk and drug interactions could worsen bleeding.
-
Gather medical history—allergies, ongoing prescriptions, and prior conditions—to expedite care once paramedics arrive.
Consequently, these steps buy crucial minutes, giving neurosurgeons and pediatric intensivists a better chance of limiting damage caused by Hemorrhagic Stroke for Health.
Diagnostic Pathway and Modern Treatments
Upon hospital arrival, the multidisciplinary stroke team proceeds briskly yet methodically. Initial CT or MRI scans not only confirm bleeding but also pinpoint its location and size. Moreover, CT angiography frequently detects vascular malformations requiring urgent neurosurgical repair. After imaging, blood tests evaluate clotting status, while, in parallel, pediatric critical care specialists stabilize airway, breathing, and circulation.
Treatment options vary, yet they usually include:
-
Surgical evacuation of hematomas to relieve pressure.
-
Endovascular coiling or stenting for treatable aneurysms.
-
Factor replacement therapies for clotting disorders.
-
Targeted blood‑pressure control using age‑appropriate intravenous medications.
Furthermore, rehabilitation starts astonishingly early. Physical, occupational, and speech therapists often join the care team within days, thereby minimizing secondary complications. Although the road is long, many children recover most functions, especially when intervention occurs promptly after a Hemorrhagic Stroke for Health.
Prevention and Long‑Term Care: Looking Beyond the Crisis
Even after discharge, vigilance continues. Therefore, regular follow‑up imaging ensures repaired vessels remain stable, while neuropsychological assessments track learning and emotional development. Families can take additional protective measures:
-
Prioritize helmet use during cycling and contact sports.
-
Keep vaccinations current to reduce infection‑related risks.
-
Manage chronic illnesses diligently; for instance, ensure sickle‑cell treatments continue on schedule.
-
Adopt heart‑healthy diets low in salt and rich in nutrients—habits that, moreover, benefit the whole household.
Furthermore, support groups and counseling help families cope with lingering anxiety. Given that psychological resilience improves adherence to therapy, fostering a positive home environment ultimately reinforces physical healing for children recovering from Hemorrhagic Stroke for Health.
Conclusion: Coordinated Care Makes the Difference
In summary, while pediatric brain bleeds remain rare, heightened awareness, swift action, and comprehensive follow‑through dramatically elevate survival odds and quality of life. Moreover, modern medicine continues to refine minimally invasive techniques, genetic testing, and personalised rehabilitation strategies, ushering in renewed hope. If your newborn experienced Perinatal Stroke or if a teenager suffered a traumatic bleed, remember that timely referral to a centre specialising in pediatric neurology ensures cutting‑edge evaluation as well as compassionate family support. Ultimately, by recognising the earliest whispers of Hemorrhagic Stroke for Health, acting decisively during that harrowing first hour, and committing to diligent long‑term care, we collectively transform outcomes for our youngest, most vulnerable patients.